Trigeminal Neuralgia
I am passionate about treating trigeminal neuralgia and other facial pain disorders, and I am a member of the Facial Pain Association. Below is an introduction to trigeminal neuralgia. You can read more about other facial pain disorders here.
If you live near Denver and have facial pain, please consider meeting me in consultation to learn about treatment options. Click here to read the information packet I provide to new patients who are seeing me for trigeminal neuralgia.
-
Trigeminal neuralgia (TN) is a common neurologic disorder in which there are lightning-like zaps of pain in the face. The pain can be excruciating, and TN is one of the most painful conditions known to man. The pain usually affects the cheek or jaw on one side of the face, and it is commonly triggered by touching the face, chewing, talking, shaving, brushing the teeth, cold air, or even a light breeze. Some patients may have more constant pain over the face rather than intermittent zaps - especially later in the disease course.
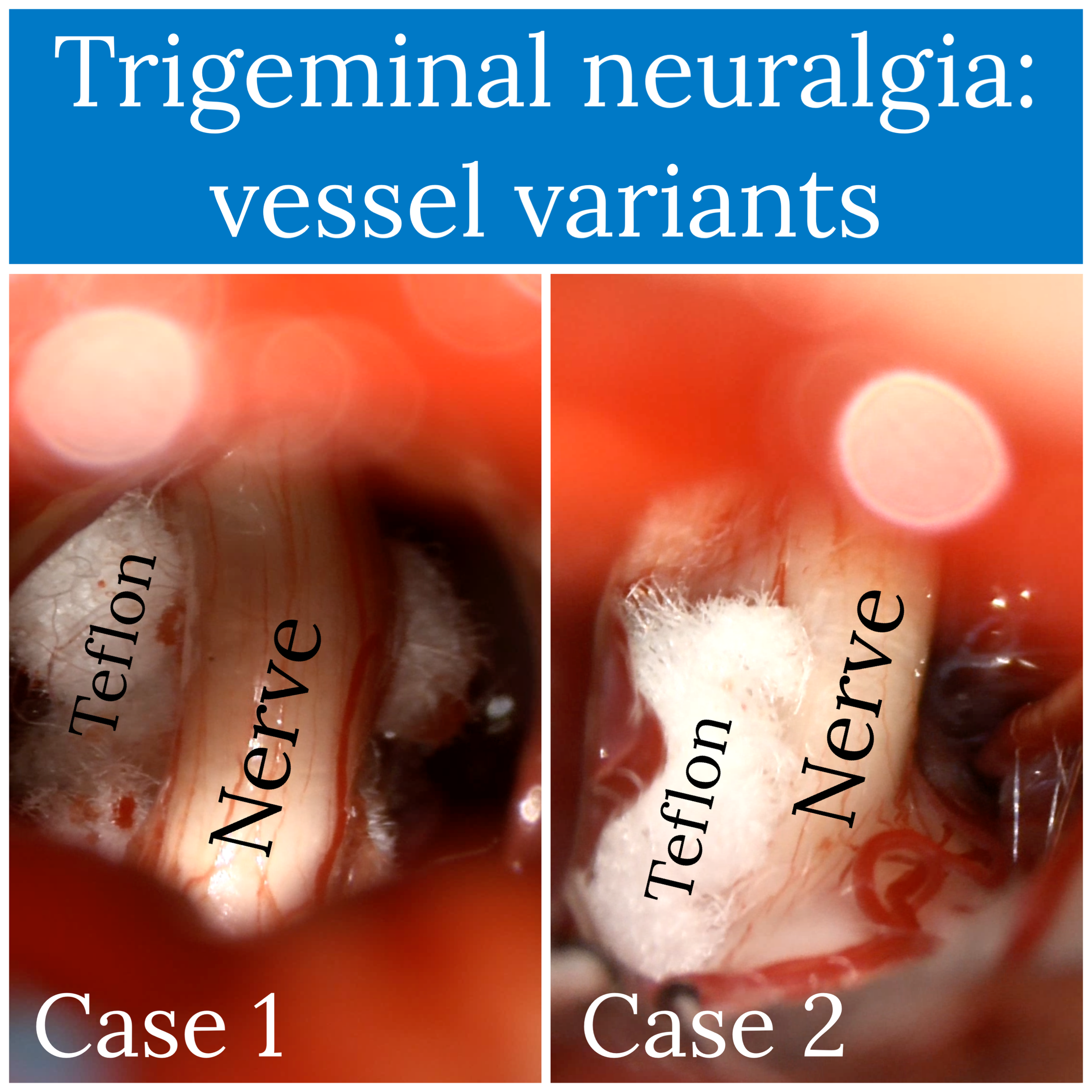
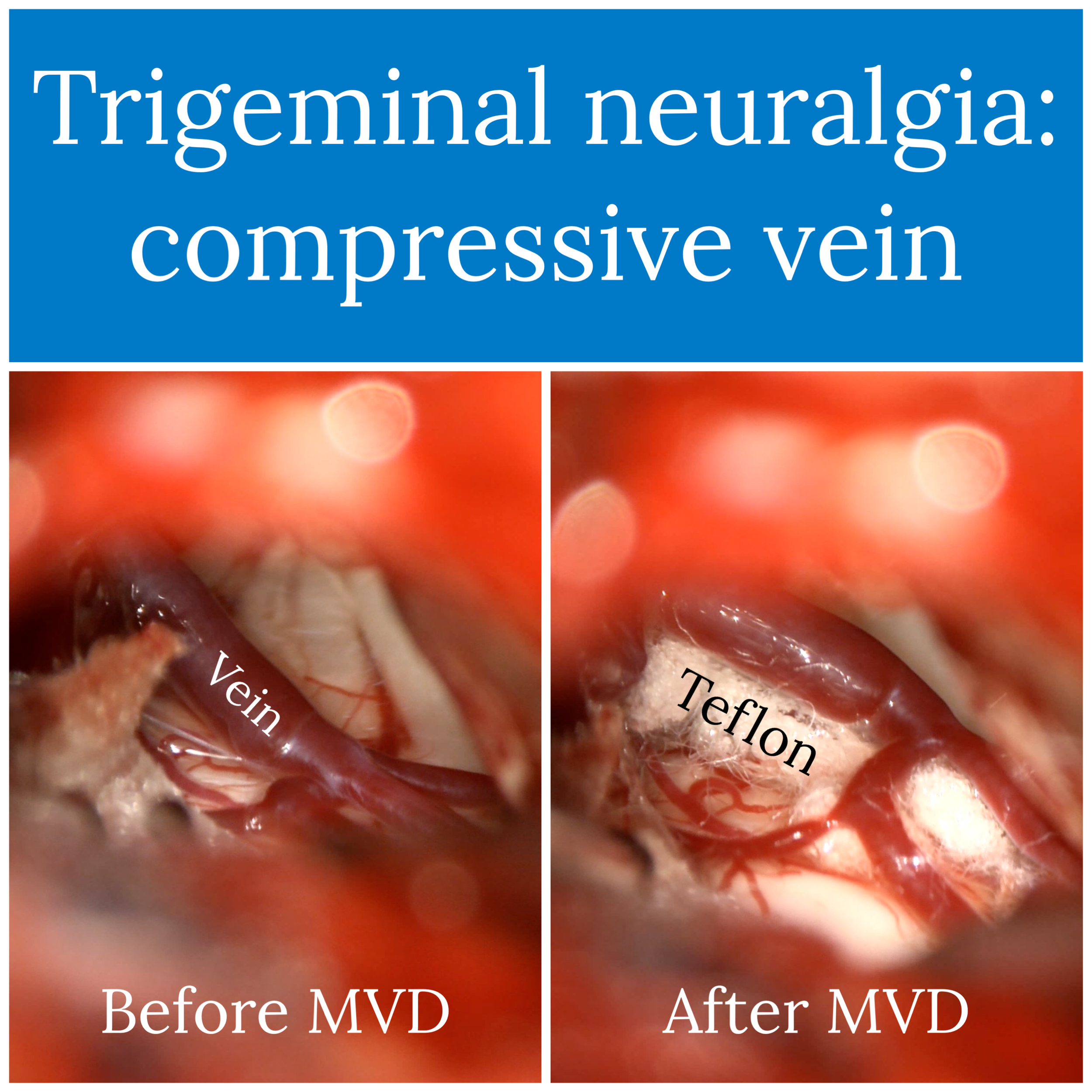
The trigeminal nerve provides sensation to the face. Patients with TN are often found to have compression of the trigeminal nerve by a blood vessel. Each time the heart beats, the blood vessel bounces against the nerve, eventually irritating the nerve and causing it to misfire. This misfiring of the nerve results in the perception of normal sensations (touch, talking, etc.) as being very painful. One of the common surgical treatments for TN, microvascular decompression, involves dissecting the blood vessel away from the trigeminal nerve and inserting a piece of padding between them.
Initial treatment for TN consists of medications, including carbamazepine (Tegretol), oxcarbazepine (Trileptal), lamotrigine (Lamcital), baclofen, and others. For patients who continue to have bothersome pain despite medication, there are several excellent surgical options, described in more detail below.
Status trigeminus refers to an acute exacerbation of trigeminal neuralgia, and it can be a medical emergency. I discuss the disorder separately here.
-
The diagnosis of trigeminal neuralgia is clinical, meaning I will review your symptoms and perform a physical exam. There is no X-ray or blood test for diagnosing trigeminal neuralgia. The clinical history in trigeminal neuralgia is critical, since TN can be mistaken for similar facial pain disorders like glossopharyngeal neuralgia, geniculate neuralgia, and trigeminal neuropathic pain, among others. It is important to find a surgeon who is familiar with these conditions.
As part of your evaluation, I will order an MRI of your brain, but this is intended to determine whether there is anything unusual causing your trigeminal neuralgia (examples: a brain tumor, multiple sclerosis) and to outline treatment options. It is your history and exam - not the MRI - that determines whether or not you have trigeminal neuralgia.
Treatment begins with medications. The most common first-line medications are carbamazepine (Tegretol) and oxcarbazepine (Trileptal). If these are not effective or cause side effects, there are several other drugs available. Opioids are generally not preferred for TN. If you have not trialed the preferred medications yet, I may refer you to one of my neurologist partners to start the process.
If the pain from TN is unbearable despite trials of two or more medications, a patient should be evaluated for surgery. There are several surgeries for TN; first-line options include microvascular decompression, trigeminal rhizotomy (radiofrequency, balloon, or alcohol), and radiosurgery. I perform all of these. Each has advantages and disadvantages. Deciding between them requires a thoughtful discussion.
-
To be considered for surgery, you should have ongoing, severe pain despite trials of at least two different medications for trigeminal neuralgia. And the medications you have tried should include either carbamazepine (Tegretol) or oxcarbazepine (Trileptal).
-
No. The MRI sometimes does not show a compressive blood vessel. Many patients with “negative” MRIs are ultimately found to have a compressive blood vessel at surgery. I routinely treat such patients, and I have seen excellent outcomes. Further, many people without any facial pain symptoms who have MRIs performed for other reasons are noticed to have blood vessels touching one of their trigeminal nerves. MRIs are not perfect!
The purpose of the MRI is to make sure there is not a tumor, multiple sclerosis, or another cause for your symptoms that would be treated in a different way. The absence of a compressive blood vessel should not automatically disqualify a patient from a microvascular decompression - or any of the other procedures I describe here.
-
Probably. TN is a lifelong condition, and symptoms can return even if they have disappeared for years. Some patients may need several different treatments over a lifetime. If you still have bothersome symptoms despite medications, you should schedule an appointment to learn more. There is value in seeing a provider who treats a high volume of TN patients like myself or another member of the Facial Pain Association.
-
Probably. I treat a wide variety of facial pain disorders that are less common than TN. Examples include occipital neuralgia, glossopharyngeal neuralgia, trigeminal neuropathic pain, and others. And TN symptoms can change over time - especially if you have previously had surgery. The best way to learn about your options is to schedule a visit with me or another provider who specializes in facial pain. You can find information about referring to my clinic here.
-
Keep track of your symptoms for a few weeks. Think about the questions listed below. These help me understand your condition and your treatment options.
* When did your pain start?
* What medications and/or surgeries have you tried?
* What does the pain feel like? (e.g. stabbing, shocking, burning, etc)
* Where in your face do you feel the pain? (draw a picture)
* Are there triggers for the pain?
* How often do you feel the pain, and how long does it last when it comes?
* Does it consist of brief zaps/shocks/stabs or constant pain? (This is important. Treatment for pain that occurs in episodes or attacks can be different than for pain that is constant and never goes away.)
* Do you have any numbness in your face? (draw a picture)
If you or a family member is suffering from trigeminal neuralgia or another facial pain disorder and live near Denver, please consider meeting me in consultation to learn more about your treatment options. The educational packet I provide to new patients meeting me for TN can be accessed here.